Abstract
Introduction: Recent advances in novel therapies and autologous stem cell transplants (ASCT) have increased treatment options for multiple myeloma (MM) and improved overall survival (OS). Previous studies suggest that racial disparities may exist in patient access to these treatments. The present study aimed to assess racial disparities in treatment patterns and clinical and economic outcomes among patients with MM. The study focused on the comparison between Caucasians (CAU) vs African Americans (AA) and Hispanics (HISP). Other racial/ethnic groups were not included due to small sample size.
Methods: Patients with a confirmed MM diagnosis (dx) from the SEER-Medicare (2007-2013) database were included. Continuous enrollment for six months before (baseline) and at least six months after the initial MM dx date was required, unless the patient died prior to that. Treatment patterns (including time from initial MM dx to first-line (1L) therapy initiation, novel therapy [i.e., lenalidomide, pomalidomide, bortezomib, carfilzomib] initiation, and ASCT), time to first hospitalization or emergency department (ED) admission after MM dx, and healthcare costs (up to one year after MM dx), OS, and MM-specific survival (MSS) among the three racial/ethnic cohorts were evaluated. Unadjusted statistical comparisons were conducted for AA vs CAU and HISP vs CAU. In addition, multivariable regression models were used to adjust for baseline characteristics, including age, gender, marital status, region, poverty indicator, MM dx year, select comorbidities, and baseline healthcare costs. Trends in novel treatment utilization and OS across MM dx years were assessed using linear regression models.
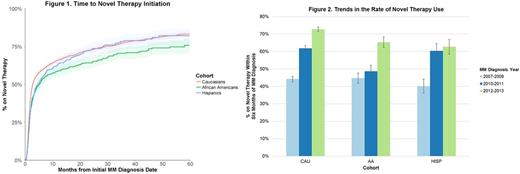
Results: The study included 4,830 patients (3,504 CAU, 858 AA, and 468 HISP). CAU were significantly older (mean age 76 years) than AA (72) and HISP (73). The average follow-up time was 2.2 years. Median time from MM dx to 1L therapy initiation was significantly longer for AA compared to CAU (1.9 vs 1.5 months, p < 0.001) and was comparable for HISP and CAU (1.8 vs 1.5 months); after adjustment, AA were less likely to initiate 1L therapy compared to CAU (hazard ratio [HR] = 0.9, p < 0.05). There was no significant difference between HISP and CAU in terms of time to initiate 1L therapy. AA and HISP also had a longer time from MM dx to novel therapy initiation compared to CAU (median: 5.2 and 4.6 vs 2.7 months; adjusted HR [AA vs CAU] = 0.8, adjusted HR [HISP vs CAU] = 0.9, both p < 0.05) (Figure 1). Around 10% of patients had an ASCT within 3 years after MM dx. HISP were less likely to receive an ASCT than CAU (3-year ASCT rate: 6.9% [HISP], 10.3% [CAU]; adjusted HR = 0.6, p < 0.05). There was no significant difference between AA and CAU (3-year ASCT rate: 7.5% vs 10.3%). Between 2007 and 2013, an increasing trend of novel therapy use within six months of MM dx was observed for all racial/ethnic groups (p < 0.05); the trend was significantly more pronounced in CAU compared to AA (p < 0.05) while similar for HISP and CAU (Figure 2).
In terms of resource utilization, AA had a significantly higher risk of ED admission compared to CAU (3-month ED admission rate: 31.2% [AA], 23.8% [CAU]; adjusted HR = 1.2, p < 0.01). Average all-cause inpatient, medical, and total costs were significantly higher among HISP than CAU (adjusted differences [HISP-CAU] $1,771, $1,651, and $1,781; p < 0.01, p < 0.05, and p < 0.01) and were comparable between AA and CAU. Median OS was comparable among the three cohorts. Median MSS was significantly longer for AA than CAU (5.4 vs 4.5 years, p < 0.05) and was comparable for HISP and CAU (4.9 vs 4.5 years). After adjustment, the risk of death due to MM remained significantly lower for AA compared to CAU (HR = 0.8, p < 0.05). No difference in OS trends were observed between racial/ethnic groups.
Conclusions: Significant variations in terms of treatment patterns and outcomes were observed among different racial/ethnic groups. While OS was similar across cohorts, both AA and HISP may not be reaping the full benefits from the introduction of novel therapies, as they receive them later than CAU. Use of novel therapy increased over time, but the increase was more pronounced in CAU than AA. Healthcare costs were similar between AA and CAU, while HISP had higher total costs than CAU, mainly driven by higher hospitalization costs. These disparities must be addressed for equitable healthcare utilization and universal benefit.
Ailawadhi: Takeda: Consultancy, Honoraria; Amgen: Consultancy, Honoraria; Pharmacyclics: Research Funding; Novartis: Consultancy, Honoraria. Parikh: Celgene Corporation: Employment. Zhou: Analysis Group, Inc.: Employment; Celgene Corporation: Other: I am an employee of Analysis Group, which received consulting fees from Celgene for this study. Tang: Analysis Group, Inc.: Employment; Celgene Corporation: Other: I am an employee of Analysis Group, which received consulting fees from Celgene for this study. Clancy: Celgene Corporation: Employment. Cheung: Analysis Group, Inc.: Employment; Celgene Corporation: Other: I am an employee of Analysis Group, which received consulting fees from Celgene for this study. Zhou: Analysis Group, Inc.: Employment; Celgene Corporation: Other: I am an employee of Analysis Group, which received consulting fees from Celgene for this study. Xie: Analysis Group, Inc.: Employment; Celgene Corporation: Other: I am an employee of Analysis Group, which received consulting fees from Celgene for this study. Abouzaid: Celgene Corporation: Employment, Equity Ownership, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal